Mental health includes our emotional, psychological, and social well-being. It affects how we think, feel, and act. It also helps determine how we handle stress, relate to others, and make choices.

At Erie, our psychiatric providers are devoted to the diagnosis, treatment, and prevention of mental, emotional, and behavioral health disorders.
Psychiatric services can only be offered to current patients who receive medical services from Erie. If you are interested in receiving psychiatric services, please talk to your Erie healthcare provider. A referral to psychiatry is not guaranteed.
Our psychiatric providers may prescribe you medication to help you feel better and cope with daily stressors. It is important to stay on your medication as advised by your provider. Learn more about refilling your medications below.
Refilling Your Psychiatric Medication
During your visit with a provider, you should be prescribed a quantity of medication to last until your next visit. When a new medication or dose is being used, you might only get enough medication for 30 days with zero additional refills. If that’s the case, you should schedule an appointment to discuss changes with your provider prior to receiving a refill.
The label of your prescription bottle can offer helpful information regarding refills.
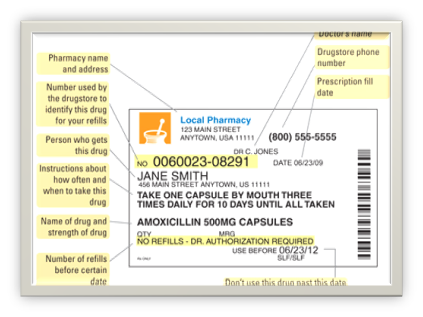
If the label says, ‘no refills,’ you’ll need to speak with your provider. This is best done by scheduling or attending your follow-up visit. It’s important to attend follow-up visits when you’re receiving a medication so you can discuss any concerns you might have about side effects or benefits of the medication. If you already have an appt coming up, great! Your provider will address the refill at the visit.
First, check your rx bottle to see if any additional refills are available.
If no refills remain, let your provider know that you’re running out before the visit.
Let the pharmacist know what medication was discussed at your visit and that it wasn’t dispensed. If the pharmacist doesn’t see the medication in the system, contact your provider to let them know the pharmacy hasn’t received the prescription so they can send it again. It’s important to pick-up and start taking your medication prior to your next visit so you can discuss with your provider how it’s going.
It sounds like they’re talking about a ‘prior authorization’ (PA). This means the medication is not on your insurance’s ‘formulary’ and your provider needs to complete documents that explain to the insurance why they think it’s best for you to take this prescription instead of a formulary medication. In many cases, your provider will already know that a PA is needed, and they might have mentioned to you that they’re already addressing it. Erie Pharmacy Services team will work on the prior authorization. Please allow 3-5 business days for processing and approval. The pharmacy will let you know the medication is now covered. If a PA wasn’t discussed at your visit, let your provider know that a PA is needed.
This can happen for several reasons. Be sure to ask why. Here are some common examples:
-
- This prescription needs a ‘prior authorization’ (PA).
- It is too early for a refill. Typically, medications cannot be refilled sooner than once every 30 days.
- You are out of refills. This might be because an appointment is needed or was missed. If you think you should still be taking the medication, check with your provider about getting a refill.
- If you have insurance, make sure the pharmacy has it on file and applied insurance coverage. Let them know if your coverage has changed.
- Next, ask if a 'prior authorization’ is needed. If a medication is not on ‘formulary’ with an insurance, it will need a prior authorization (PA) in order to get it covered by the insurance.
- If you don’t have insurance or your insurance does not cover the medication, use a Walgreens Pharmacy and ask about the “340B discount” – this might make the medication affordable. Walgreens also offers a “Prescription Savings Club” for an annual fee that may reduce the cost.
- If none of the above options are making the medication affordable for you, call Erie Family Health Center at 312-666-3494 and select the option for prescription refills. The Pharmacy Services team is dedicated to assisting troubleshooting issues with medication.
It can be uncomfortable to take a medication when you don’t know what it’s for. Usually, the provider who prescribed the medication will have discussed this with you. If you don’t remember the discussion, look at the prescription bottle – it will usually say why the medication is being prescribed. You can also log into MyChart and check the notes from your last provider visit to better understand why a particular medication was prescribed.
This is a common concern. The medications that we often refer to as ‘antidepressants’ are actually also recommended for treating anxiety! This is because a lot of the same neurotransmitters (eg, serotonin, dopamine, norepinephrine) are involved in symptoms of depression and anxiety.
That depends! Some medications must be taken consistently every day in order to be effective. Other medications are ‘PRN’ which means they are meant to be taken ‘as needed.’ If you don’t remember the instructions discussed by your provider, take a look at the rx bottle.

An example of medications that MUST be taken daily in order to be beneficial is the selective serotonin reuptake inhibitor (SSRI) and selective serotonin norepinephrine reuptake inhibitor (SNRI) medications. These are often used for depression and for anxiety. Common SSRIs include: fluoxetine (Prozac), sertraline (Zoloft), paroxetine (Paxil), escitalopram (Lexapro), and citalopram (Celexa). Common SNRIs include: venlafaxine (Effexor), duloxetine (Cymbalta), and desvenlafaxine (Pristiq).
If it’s a non-controlled substance, no problem! Just ask the pharmacy to transfer the prescription to the other location. This can be done easily if you’re transferring to a different location for the same chain pharmacy (eg, one Walgreens location to another, or one CVS location to another).
If it’s a controlled substance, a new prescription must be requested from your provider to send directly to that pharmacy. Controlled substances cannot be transferred between pharmacies.
Have your prescription sent to a chain pharmacy that is located in Illinois. Our providers are licensed to prescribe in Illinois and cannot send prescriptions out of the state, but non-controlled substances can be transferred to the same chain pharmacy at a different location.
If it is a controlled substance, unfortunately, we cannot send the prescription out of state, and it cannot be transferred between pharmacies. You will need to ensure you fill your prescription while you are still in the state or wait until you return.
Make sure you get adequate refills prior to leaving since we cannot send prescription refills outside of the country. If you need refills while out of the country, you will have to visit a provider in that country to address the refill.
Call (312) 666-3494 to schedule an appointment.
For our suburban locations call (847) 666-3494

Erie Family Health Centers received the USA Today Top Workplaces 2024 Award and the Top Workplaces 2024 Purpose and Values Award, recognizing that our shared belief in Erie's mission and values drives everything we do.
